Naghmeh Bandari received her Bachelor’s and Master’s degrees in biomedical engineering from Amirkabir University of Tehran, Iran, where she served as a Certified Medical Device Technical Supervisor for six years. She is a doctoral candidate of Mechanical Engineering at the Optical-Bio-MEMS and Robotic Surgery Labs. She is also a fellow of Surgical Innovation at the Natural Sciences and Engineering Research Council of Canada (NSERC) CREATE program for Innovation-at-the-Cutting-Edge (ICE). Her research focuses on the development of optical tactile sensors and micro-optical mechanical systems for robotic and surgical applications.
Blog post
Tactile sensors improve surgical success and patient safety in treating cardiac arrhythmia
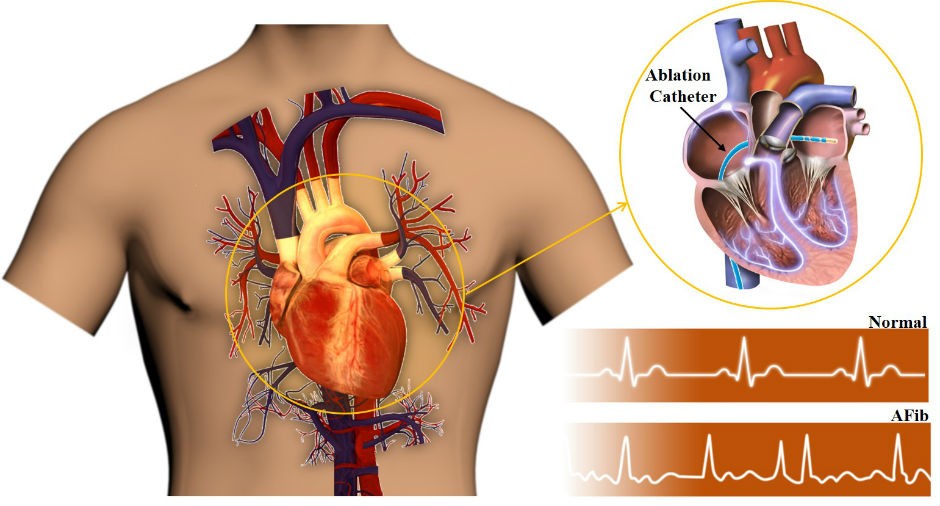 A normal heartbeat versus an AFib heartbeat, along with minimally invasive ablation catheter treatment.
A normal heartbeat versus an AFib heartbeat, along with minimally invasive ablation catheter treatment.
Open surgery is often associated with blood loss, pain, infection, prolonged recovery time and complications. Minimally invasive surgery (MIS), however, allows the surgeon to reach the internal organs of the patient through small skin incisions as small as five millimetres. In MIS, the surgeon utilizes long and slender surgical instruments to enter the body’s cavities, arteries and organs like the heart, liver and brain, without needing to cut open the body.
One of the most frequently used instruments in MIS is the catheter, which is a long flexible hollow tube. Surgeons use catheters mainly in heart and artery surgeries. For example, surgeons employ catheters to treat one of the most prevalent cardiac diseases known as atrial fibrillation (AFib).
AFib is a medical condition that causes the heart to beat slower or faster than normal. AFib is the leading cause of stroke among people 65 years and older. Estimates show that this disease affects nearly 20 million people worldwide. When AFib is untreated, it may lead to valve degeneration, sleep apnea, fatigue, heart failure and, eventually, a stroke.
Studies show that AFib starts when some of the pulses that generate cells in our heart become hyperactive, causing faster beating, or lazy, causing slower beating. I simply call those cells as rogue cells.
Treatment: radio-frequency cardiac ablation
Now, if you are wondering how grilling might relate to the treatment of AFib in surgery, I would say that the treatment of AFib — known as radiofrequency ablation — is nothing but burning the rogue cells using microwave radiation, just like melting cheese or grilling a steak on an induction grill. Srijoy Mahapatra, chief strategy officer at Fairview Health Services, first used the grilled cheese metaphor.
In the case of a thick steak, one may prefer to press down on the steak with a spatula so that it gets grilled deep inside. The same process happens in burning cells inside the patient’s heart. Surgeons aim to burn all the rogue cells but not to overcook the heart wall — which would result in puncturing the heart and is the last thing a patient needs on the operating table.
The success of AFib treatment strongly depends on the pressure between the ablation device — catheter — and the heart wall where the rogue cells reside. Universities and industry developed several technologies to monitor this pressure with contact sensing technology. Such sensors are generally known as tactile sensors, which are embedded at the tip of the ablation catheters.
My PhD research has been on developing such tactile sensors for various cardiac surgeries, like valve replacement, angioplasty, stent placement and AFib treatment. One of the most essential properties of such sensors is that they must be tiny — less than six millimetres in diameter. Also, these sensors must be radio-silent so that they do not affect or interfere with other devices in the operation room.
Most importantly, the electrical activity of the heart must not affect the performance of such a sensor.
Sensor technology for optimal clinical success
The surgical tactile sensors proposed by researchers are designed based on electrical or optical sensing methods. Electrical tactile sensors mainly employ variable capacitance, piezoelectricity and piezo-resistivity phenomena. Electrical sensors possess simple sensing principles, are capable of direct force measurement and are scalable to different lengths. However, these properties have led researchers to use such sensors in MIS applications where MR-compatibility is not a clinical priority.
On the other hand, optical-based sensors satisfy MR-compatibility, electro-passivity and size; thus, they make the right choice in MIS applications. Besides, sterilizability, integrability and low-cost production are remarkable advantages of the optical-based sensors.
During the past decade, catheter technologies have been enhanced with tactile sensor integration. Manipulating a catheter in the heart during MIS to burn the rogue cells is somewhat like threading a needle without seeing the needle. One would need many trials and errors and would rely on their sense of touch to find the hole, let alone pass the thread. It’s nearly impossible, no?
The launch of TactiCath™ Ablation Catheter, Sensor Enabled™ produced by former St. Jude Medical Inc. — now Abbot Medical Inc. — in October 2014 made precise catheter manipulation with sensing technology possible. The embedded sensor works based on optical principles. Indeed, optical fibers bring the contact force information from the catheter's tip to the surgeon’s hand. Then, an open system with 3D visualization provides surgeons with a real-time mapping model of the heart.
 TactiCath™ Ablation Catheter, Sensor Enabled™, Abbot Medical Inc. | Courtesy of Abbot Medical Inc.
TactiCath™ Ablation Catheter, Sensor Enabled™, Abbot Medical Inc. | Courtesy of Abbot Medical Inc.
In August 2016, Biosense Webster Inc. introduced another sensorized catheter named ThermoCool® SmartTouch® after stringent reviews and certification by the U.S. Food and Drug Administration.
The picture below shows the SmartTouch® catheter with a sensor at its tip. The sensor on this catheter is a tactile sensor that rapidly and precisely measures the force the catheter applies on the heart wall so that the surgeon burns the rogue cells while keeping the correct contact pressure.
Studies show that this technology decreases the length of surgeries by almost 20 per cent. That’s a huge success. Also, it reduces X-ray exposure — used to see inside the patient’s heart during the surgery — by 55 per cent.
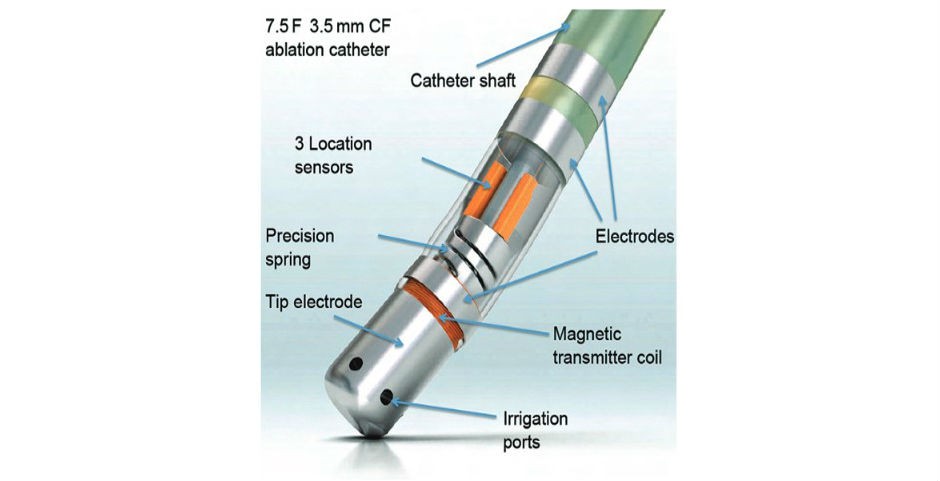 ThermoCool® SmartTouch®, Biosense Webster Inc., CA, US. | Lin et al., Arrhythmia & Electrophysiology Review 2013; 3 (1): 44-7.
ThermoCool® SmartTouch®, Biosense Webster Inc., CA, US. | Lin et al., Arrhythmia & Electrophysiology Review 2013; 3 (1): 44-7.
In the end, the sense of touch is invaluable during modern surgery. Compensating for that loss is of prime importance. Technologies like tactile sensors enhance the safety of operations for patients, reduce the costs of care for governments, push the boundaries of knowledge and, ultimately, contribute to the general well-being of the public by saving lives.
About the author


